Plus get our latest book recommendations, author news, and competitions right to your inbox.
Table of Contents
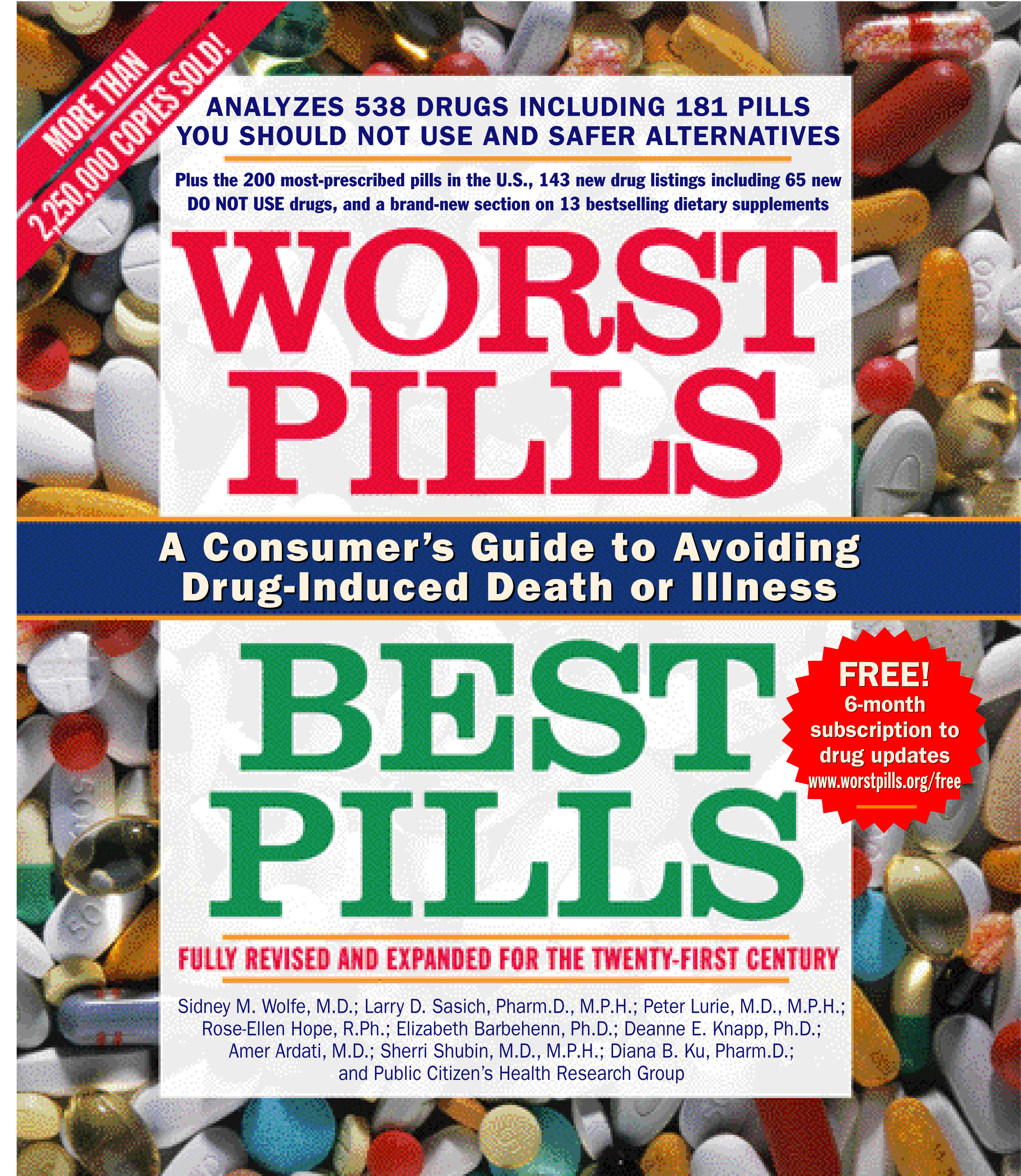
About The Book
"More than 100,000 people a year die in American hospitals from adverse reactions to medication, making drug reactions one of the leading causes of death in this country, researchers are reporting today...."
-- Journal of the American Medical Association study, as quoted in The New York Times
It is no longer a secret that adverse drug reactions can be dangerous or even fatal, or that doctors often prescribe two relatively safe drugs -- which may cause a life-threatening interaction if taken together. THIS IS THE BOOK THAT TELLS YOU WHAT OTHER PILL BOOKS WON'T ABOUT YOUR MEDICATION!
Top-selling drugs that are among the 160 Do Not Use Drugs discussed inside:
Consumer advocate Sidney M. Wolfe, M.D., director of Public Citizen's Health Research Group, has thoroughly revised and updated this accessible, indispensable bestseller that alerts you to the potential risks of hundreds of medications available today. Worst Pills, Best Pills gives you the information you need to become actively involved in caring for yourself -- by asking your doctor smart questions about the drugs prescribed for you. Arranged by disease/condition, it offers chapters on adverse drug reactions, alphabetical indexes listing pills by their brand and generic names, new information about commonly used drugs, guidelines for helping you to say "no" if your doctor prescribes a drug you should not take, and safer alternative choices. Worst Pills, Best Pills also includes startling information about certain drugs that can actually cause depression, hallucinations or psychoses, sexual dysfunction, dementia, auto accidents, insomnia, parkinsonism, and more.
Caution: Call your doctor before stopping the use of any drug.
-- Journal of the American Medical Association study, as quoted in The New York Times
It is no longer a secret that adverse drug reactions can be dangerous or even fatal, or that doctors often prescribe two relatively safe drugs -- which may cause a life-threatening interaction if taken together. THIS IS THE BOOK THAT TELLS YOU WHAT OTHER PILL BOOKS WON'T ABOUT YOUR MEDICATION!
Top-selling drugs that are among the 160 Do Not Use Drugs discussed inside:
- Ultram
- Darvoset-N
- Lopid
- Desogen & OrthoCept
- Elavil
- Ativan
- Restoril
- Flexeril
- Valium
- Bentyl
- Entex LA
- Glucophage
- Macrobid
Consumer advocate Sidney M. Wolfe, M.D., director of Public Citizen's Health Research Group, has thoroughly revised and updated this accessible, indispensable bestseller that alerts you to the potential risks of hundreds of medications available today. Worst Pills, Best Pills gives you the information you need to become actively involved in caring for yourself -- by asking your doctor smart questions about the drugs prescribed for you. Arranged by disease/condition, it offers chapters on adverse drug reactions, alphabetical indexes listing pills by their brand and generic names, new information about commonly used drugs, guidelines for helping you to say "no" if your doctor prescribes a drug you should not take, and safer alternative choices. Worst Pills, Best Pills also includes startling information about certain drugs that can actually cause depression, hallucinations or psychoses, sexual dysfunction, dementia, auto accidents, insomnia, parkinsonism, and more.
Caution: Call your doctor before stopping the use of any drug.
Excerpt
CHAPTER ONE
MISPRESCRIBING AND OVERPRESCRIBING OF DRUGS: Evidence and Causes
The numbers are staggering: in 1997, an estimated 2.35 billion prescriptions were filled in retail drugstores in the United States. For those people who got at least one prescription filled, this amounts to an average of 11.6 prescriptions per person that year.
There is no dispute that for many people, prescriptions are beneficial, even lifesaving in many instances. But hundreds of millions of these prescriptions are wrong, either entirely unnecessary or unnecessarily dangerous. At the very least, misprescribing wastes tens of billions of dollars, barely affordable by many people who pay for their own prescriptions. But there are much more serious consequences. More than 1.5 million people are hospitalized and more than 100,000 die each year from largely preventable adverse reactions to drugs that should not have been prescribed as they were in the first place. What follows is a summary of the seven all-too-often-deadly sins of prescribing.
First: The "disease" for which a drug is prescribed is actually an adverse reaction to another drug, masquerading as a disease but unfortunately not recognized by doctor and patient as such. Instead of lowering the dose of the offending drug or replacing it with a safer alternative, the physician adds a second drug to the regimen to "treat" the adverse drug reaction caused by the first drug. Examples discussed in this book include drug-induced parkinsonism, depression, sexual dysfunction, insomnia, psychoses, constipation, and many other problems.
Second: A drug is used to treat a problem which, although in some cases susceptible to a pharmaceutical solution, should first be treated with common sense lifestyle changes. Problems such as insomnia and abdominal pain often have causes that respond very well to nondrug treatment, and often the physician can uncover these causes by taking a careful history. Other examples include medical problems such as high blood pressure, mild adult-onset diabetes, obesity, anxiety, and situational depression. Doctors should recommend lifestyle changes as the first approach for these conditions, rather than automatically reach for the prescription pad.
Third: The medical problem is both self-limited and completely unresponsive to treatments such as antibiotics or does not merit treatment with certain drugs. This is seen most clearly with viral infections such as colds and bronchitis in otherwise healthy children or adults.
Fourth: A drug is the preferred treatment for the medical problem, but instead of the safest, most effective -- and often least expensive -- treatment, the physician prescribes one of the 160 Do Not Use drugs listed in this book or another, much less preferable alternative. An example of a less preferable alternative would be a drug to which the patient has a known allergy that the physician did not ask about.
Fifth: Two drugs interact. Each on its own may be safe and effective, but together they can cause serious injury or death.
Sixth: Two or more drugs in the same therapeutic category are used, the additional one(s) not adding to the effectiveness of the first but clearly increasing the risk to the patient. Sometimes the drugs come in a fixed combination pill, sometimes as two different pills. Often heart drugs or mind-affecting drugs are prescribed in this manner.
Seventh: The right drug is prescribed, but the dose is dangerously high. This problem is seen most often in older adults, who cannot metabolize or excrete drugs as rapidly as younger people. This problem is also seen in small people who are usually prescribed the same dose as that prescribed to people weighing two to three times as much as they do. Thus, per pound, they are getting two to three times as much medicine as the larger person.
Evidence of Misprescribing and Overprescribing
Here are some examples from recent studies by a growing number of medical researchers documenting misprescribing and overprescribing of drugs:
Treating Adverse Drug Reactions -- as Diseases -- with Other Drugs
Researchers at the University of Toronto and at Harvard have clearly documented and articulated what they call the prescribing cascade. It begins when an adverse drug reaction is misinterpreted as a new medical condition. Another drug is then prescribed, and the patient is placed at risk of developing additional adverse effects relating to this potentially unnecessary treatment. To prevent this prescribing cascade, doctors -- and patients -- should follow what we call Rule 3 of the Ten Rules for Safer Drug Use: Assume that any new symptom you develop after starting a new drug might be caused by the drug. If you have a new symptom, report it to your doctor.
Some of the instances of the prescribing cascade that these and other researchers have documented include:
Failing to Treat Certain Problems with Nondrug Treatments
Research has shown that many doctors are too quick to pull the prescription trigger. In one study, in which doctors and nurse practitioners were presented with part of a clinical scenario -- as would occur when first seeing a patient with a medical problem -- and then encouraged to ask to find out more about the source of the problem, 65% of doctors recommended that a patient complaining of insomnia be treated with sleeping pills even though, had they asked more questions about the patient, they would have found that the patient was not exercising, was drinking coffee in the evening, and, although awakening at 4 A.M., was actually getting seven hours of sleep by then.
In a similar study, doctors were presented with a patient who complained of abdominal pain and endoscopy showed diffuse irritation in the stomach. Sixty-five percent of the doctors recommended treating the problem with a drug -- a histamine antagonist (such as Zantac, Pepcid, or Tagamet). Had they asked more questions they would have discovered that the patient was using aspirin, drinking a lot of coffee, smoking cigarettes, and was under considerable emotional stress -- all potential contributing factors to abdominal pain and stomach irritation.
In summarizing the origin of this overprescribing problem, the authors stated: "Apparently quite early in the formulation of the problem, the conceptual focus [of the doctor] appears to shift from broader questions like 'What is wrong with this patient?' or 'What can I do to help?' to the much narrower concern, 'Which prescription shall I write?'" They argued that this approach was supported by the "barrage" of promotional materials that only address drug treatment, not the more sensible lifestyle changes to prevent the problem.
In both of the above scenarios, nurse practitioners were much more likely than doctors to take an adequate history that elicited the causes of the problems and, not surprisingly, were only one-third as likely as the doctors to decide on a prescription as the remedy instead of suggesting changes in the patient's habits.
In later discussions about insomnia, high blood pressure, situational depression, mild adult-onset diabetes, and other problems, you will find out about the proven-effective nondrug remedies that should first be pursued before yielding to the riskier pharmaceutical solutions.
Treating Viral Infections with Antibiotics or Treating Other Diseases with Drugs That Are Not Effective for Those Problems
Two recently published studies, based on nationwide data from office visits for children and adults, have decisively documented the expensive and dangerous massive overprescribing of antibiotics for conditions which, because of their viral origin, do not respond to these drugs. Forty-four percent of children under 18 years old were given antibiotics for treatment of a cold and 75% for treatment of bronchitis. Similarly, 51% of people 18 or older were treated with antibiotics for colds and 66% for bronchitis. Despite the lack of evidence of any benefit for most people from these treatments, more than 23 million prescriptions a year were written for colds, bronchitis, and upper respiratory infections. This accounted for approximately one-fifth of all prescriptions for antibiotics written for children or adults. An accompanying editorial warned of "increased costs from unnecessary prescriptions, adverse drug reactions, and [subsequent] treatment failures in patients with antibiotic-resistant infections" as the reasons to try to reduce this epidemic of unnecessary antibiotic prescribing.
Similar misprescribing of a drug useful and important for certain problems, but not necessary or effective -- and often -- dangerous for other problems can be seen in another recent study. In this case, 47% of the people admitted to a nursing home who were taking digoxin, an important drug for treating an abnormal heart rhythm called atrial fibrillation or for treating severe congestive heart failure, did not have either of these medical problems and were thereby being put at risk for life-threatening digitalis toxicity without the possibility of any benefit.
A final example in this category involves the overuse of a certain class of drugs, in this case calcium channel blockers, which have not been established as effective for treating people who have had a recent heart attack. The study shows that this prescribing pattern actually did indirect damage to patients because their use was replacing the use of beta-blockers, drugs shown to be very effective for reducing the subsequent risk of death or hospitalization following a heart attack. Use of a calcium channel blocker instead of a beta-blocker was associated with a doubled risk of death, and beta-blocker recipients were hospitalized 22% less often than nonrecipients.
The Prescribing of More Dangerous and/or Less Effective Do Not Use Drugs Instead of Safer Alternatives
There are 160 drugs listed in this book for which we recommend safer alternatives. Forty-three of these Do Not Use drugs are for heart disease or high blood pressure and make up 39% of all the drugs in the book for these problems. Twenty of the Do Not Use drugs are for treating insomnia, anxiety, depression, or other mental problems, and make up 43% of the drugs in the book for these problems. Another 20 of the Do Not Use drugs are for treating pain, and make up 36% of the drugs in the book for these problems. Thirteen of the Do Not Use drugs are for treating gastrointestinal problems and make up 37% of the drugs in the book for these problems. Twenty-four of the Do Not Use drugs are for treating coughs, colds, allergies, or asthma, and make up 63% of the drugs in the book for these problems. Sixteen of the Do Not Use drugs are for treating infections and make up 28% of the drugs in the book for these problems. Although the original determinations for these Do Not Use drugs were based on their use by older adults, we have concluded that the same warnings apply to use by any adults.
Included in this list of 160 are drugs we label Do Not Use Until Five Years After Release. We have applied this warning to drugs that have only recently appeared on the market, for which there is no evidence of their superiority over older drugs about which we have much more information as to long-term safety and effectiveness. Because of incomplete and worrisome safety information, there is a risk that some of these newer drugs will have to be banned. But by the time they have been on the market for five years, it is much less likely that they will be banned, and it is much more likely that, if they are still being used, there will be much better information about their safety and effectiveness.
Another category of drugs that is misprescribed even though there are safer alternatives, are drugs to which patients are known to be allergic, but which their physicians have not taken a careful medical history about.
The Causes of Misprescribing and Overprescribing: Drug Companies, the FDA, Doctors, Pharmacists, and Inadequately Informed or Not-Vigilant-Enough Patients
The Drug Industry
The primary culprit in promoting the misprescribing and overprescribing of drugs is the pharmaceutical industry, which now sells about $80 billion worth of drugs in the United States alone. By intimidating the Food and Drug Administration (FDA) into approving record numbers of me-too drugs (drugs that offer no significant benefit over drugs already on the market) that often have dangerous adverse effects and by spending well in excess of $12 billion a year to promote drugs, using advertising and promotional tricks that push at or through the envelope of being false and misleading, this industry has been extremely successful in distorting, in a profitable but dangerous way, the rational processes for approving and prescribing drugs. Two studies of the accuracy of ads for prescription drugs widely circulated to doctors both concluded that a substantial proportion of these ads contained information that was false or misleading and violated FDA laws and regulations concerning advertising.
The fastest-growing segment of drug advertising is directed not at doctors but at patients. It has been estimated that from 1991 to 1998, DTC (direct-to-consumer) advertising expenditures in the United States grew from about $60 million a year to $1.5 billion a year, an increase of 25-fold in just seven years, employing misleading advertising campaigns similar to those used for doctors. A recent study by Consumer Reports of 28 such ads found that "only half were judged to convey important information on side effects in the main promotional text," only 40% were "honest about efficacy and fairly described the benefits and risks in the main text," and 39% of the ads were considered "more harmful than helpful" by at least one reviewer. This campaign has been extremely successful. According to a drug industry spokesman, "There's a strong correlation between the amount of money pharmaceutical companies spend on DTC advertising and what drugs patients are most often requesting from physicians." The advertising "is definitely driving patients to the doctor's office, and in many cases, leading patients to request the drugs by name." The problems with DTC advertising are best summed up in an article written by a physician ten years ago in The New England Journal of Medicine, before the current binge had really begun: "If direct [to consumer] advertising should prevail, the use of prescription medication would be warped by misleading commercials and hucksterism. The choice of a patient's medication, even of his or her physician, could then come to depend more on the attractiveness of a full-page spread or prime-time commercial than on medical merit...such advertising would serve only the admakers and the media, and might well harm our patients."
The Food and Drug Administration (FDA)
Attempting to fend off FDA-weakening legislation even worse than that which was signed into law in 1997, the FDA has bent over backwards to approve more drugs, culminating in 1996 and 1997 when the agency approved a larger number than had ever been approved in any two-year period. Thousands of people were injured or killed after taking one of three such recently approved drugs (which have subsequently been recalled from the market). These drugs were the weight loss drug dexfenfluramine (REDLUX), a heart drug mibefradil (POSICOR), and the painkiller bromfenac (DURACT). Other drugs that would not have gotten approved in a more cautious era at the FDA have also been approved, but are likely either to be banned or to be forced to carry severe warnings that will substantially reduce their use. Many of these are included in this book and listed as Do Not Use drugs.
In the 27 years since the Public Citizen's Health Research Group started monitoring the FDA and the drug industry, the current pro-industry attitude at the FDA is as bad and dangerous as it has ever been. In addition to record numbers of approvals of questionable drugs, FDA enforcement over advertising has fallen behind. The division at FDA responsible for policing prescription drug advertising has not been given adequate resources to keep up with the torrent of newly approved drugs. As a result, the drug industry correctly believes it can get away with more violative advertising than in the past. The role of the U.S. Congress in pushing the FDA into approving more drugs, and passing, with the FDA's reluctant approval, legislation to further weaken the FDA's ability to protect the public, cannot be overlooked.
Physicians
The well-financed promotional campaigns by drug companies would not have as much of an impact as they do were there not such an educational vacuum about proper prescribing of drugs, a serious problem that must be laid at the feet of medical school and residency training. The varieties of overprescribing and misprescribing of drugs by doctors -- the seven all-too-often-deadly sins of prescribing -- are all strongly enhanced by the mind-altering properties of drug promotion. The best doctors, of whom there are many, do not waste their time talking to drug sales people, toss promotional materials away, and ignore drug ads in medical journals. Too many other doctors, however, are heavily influenced by drug companies, accepting free meals, free drinks, and free medical books in exchange for letting the drug companies "educate" them at symposia in which the virtues of certain drugs are extolled. Unfortunately, many of these doctors are too arrogant to realize that there is no such thing as a free lunch. The majority of doctors attending such functions have been found to increase their prescriptions for the targeted drugs following attendance at the "teach-in."
Beyond traditional advertising and promotion and their influence, bias of drug-company-sponsored research, as published in medical journals, also can sway doctors toward more favorable impressions about drugs. An analysis was done of 56 trials that were paid for by drug companies and reported in 52 medical journals about drugs for arthritis and pain -- non-steroidal anti-inflammatory drugs (NSAIDs). (These drug-company-sponsored studies represented 85% of those that the researchers originally looked at.) In studies identifying the company's drug as less toxic than another drug, in barely one-half of the studies was there justification for the finding of less toxicity. This certainly explains why, contrary to fact, newer arthritis drugs almost always "seem" safer than older, usually much less expensive ones.
A final example demonstrates the ignorance of many physicians, especially in dealing with prescribing drugs to older adults. A study of physicians who treat Medicare patients found that 70% of the doctors who took an examination concerning their knowledge of prescribing for older adults failed to pass the test. The majority of physicians who were contacted for participation in the study refused to take the test, often giving as their reason that they had a "lack of interest in the subject." The authors concluded "many of these physicians [who failed the exam] had...not made good use of the best information on prescribing for the elderly."
Pharmacists
A small fraction of pharmacists have, in our view, betrayed their professional ethics and are working for drug companies, engaging in such activities as calling doctors to get them to switch patients from drugs made by a company other than the one the pharmacist works for to the pharmacist's employer's drugs. In addition, pharmacy organizations such as the American Pharmaceutical Association and others have fought hard to prevent the FDA from requiring accurate patient package information to be dispensed with each prescription filled.
Too many pharmacists, despite having computers to aid them, have been willing to fill prescriptions for pairs of drugs which, because of life-threatening adverse drug interactions if used at the same time, should never be dispensed to the same person.
Patients
For too many patients, the system is stacked against you -- drug companies, doctors, and pharmacists are too often making decisions that ultimately derive from what is best for the drug companies, doctors, and pharmacists, and not necessarily from what is best for you. This book has been researched and written to help you come out ahead in the struggle with our health care industry.
In Chapter 2, concerning adverse drug reactions, you can learn which common medical problems -- depression, insomnia, sexual disorders, parkinsonism, falls and hip fractures, constipation, and many others -- can actually be caused by drugs. Once you recognize these problems, you can take care of yourself and your family and bring the problems to an end by discussing safer alternatives with your physician.
Chapter 3, the largest section of the book, discusses 456 drugs, including 160 that we and our consultants think you should not use. For each of these, we recommend safer alternatives. In addition, Chapter 3 lists hundreds of drug combinations that should not be used because of serious interactions.
Chapter 4 presents a detailed strategy, beyond information on specific adverse effects and drugs, to help you to use drugs more safely, including Ten Rules for Safer Drug Use and how to use and maintain your own Drug Worksheet for Patient, Family, Doctor and Pharmacist. This is your personalized plan for avoiding becoming a victim of overprescribing or misprescribing.
Chapter 5 discusses the latest information about generic drugs and shows you how and why you can and should save hundreds of dollars a year or more.
In short, this book is intended to help you and your family to improve your health by using drugs, if necessary, more carefully and recognizing those you should avoid.
Copyright © 1999 by Public Citizen Foundation, Inc., Sidney M. Wolfe, M.D., and the Public Citizen's Health Research Group
MISPRESCRIBING AND OVERPRESCRIBING OF DRUGS: Evidence and Causes
The numbers are staggering: in 1997, an estimated 2.35 billion prescriptions were filled in retail drugstores in the United States. For those people who got at least one prescription filled, this amounts to an average of 11.6 prescriptions per person that year.
There is no dispute that for many people, prescriptions are beneficial, even lifesaving in many instances. But hundreds of millions of these prescriptions are wrong, either entirely unnecessary or unnecessarily dangerous. At the very least, misprescribing wastes tens of billions of dollars, barely affordable by many people who pay for their own prescriptions. But there are much more serious consequences. More than 1.5 million people are hospitalized and more than 100,000 die each year from largely preventable adverse reactions to drugs that should not have been prescribed as they were in the first place. What follows is a summary of the seven all-too-often-deadly sins of prescribing.
First: The "disease" for which a drug is prescribed is actually an adverse reaction to another drug, masquerading as a disease but unfortunately not recognized by doctor and patient as such. Instead of lowering the dose of the offending drug or replacing it with a safer alternative, the physician adds a second drug to the regimen to "treat" the adverse drug reaction caused by the first drug. Examples discussed in this book include drug-induced parkinsonism, depression, sexual dysfunction, insomnia, psychoses, constipation, and many other problems.
Second: A drug is used to treat a problem which, although in some cases susceptible to a pharmaceutical solution, should first be treated with common sense lifestyle changes. Problems such as insomnia and abdominal pain often have causes that respond very well to nondrug treatment, and often the physician can uncover these causes by taking a careful history. Other examples include medical problems such as high blood pressure, mild adult-onset diabetes, obesity, anxiety, and situational depression. Doctors should recommend lifestyle changes as the first approach for these conditions, rather than automatically reach for the prescription pad.
Third: The medical problem is both self-limited and completely unresponsive to treatments such as antibiotics or does not merit treatment with certain drugs. This is seen most clearly with viral infections such as colds and bronchitis in otherwise healthy children or adults.
Fourth: A drug is the preferred treatment for the medical problem, but instead of the safest, most effective -- and often least expensive -- treatment, the physician prescribes one of the 160 Do Not Use drugs listed in this book or another, much less preferable alternative. An example of a less preferable alternative would be a drug to which the patient has a known allergy that the physician did not ask about.
Fifth: Two drugs interact. Each on its own may be safe and effective, but together they can cause serious injury or death.
Sixth: Two or more drugs in the same therapeutic category are used, the additional one(s) not adding to the effectiveness of the first but clearly increasing the risk to the patient. Sometimes the drugs come in a fixed combination pill, sometimes as two different pills. Often heart drugs or mind-affecting drugs are prescribed in this manner.
Seventh: The right drug is prescribed, but the dose is dangerously high. This problem is seen most often in older adults, who cannot metabolize or excrete drugs as rapidly as younger people. This problem is also seen in small people who are usually prescribed the same dose as that prescribed to people weighing two to three times as much as they do. Thus, per pound, they are getting two to three times as much medicine as the larger person.
Evidence of Misprescribing and Overprescribing
Here are some examples from recent studies by a growing number of medical researchers documenting misprescribing and overprescribing of drugs:
Treating Adverse Drug Reactions -- as Diseases -- with Other Drugs
Researchers at the University of Toronto and at Harvard have clearly documented and articulated what they call the prescribing cascade. It begins when an adverse drug reaction is misinterpreted as a new medical condition. Another drug is then prescribed, and the patient is placed at risk of developing additional adverse effects relating to this potentially unnecessary treatment. To prevent this prescribing cascade, doctors -- and patients -- should follow what we call Rule 3 of the Ten Rules for Safer Drug Use: Assume that any new symptom you develop after starting a new drug might be caused by the drug. If you have a new symptom, report it to your doctor.
Some of the instances of the prescribing cascade that these and other researchers have documented include:
- The increased use of anti-Parkinson's drugs to treat drug-induced parkinsonism caused by the heartburn drug metoclopramide 4 (REGLAN) or by some of the older antipsychotic drugs.
- A sharply increased use of laxatives in people with decreased bowel activity that has been caused by antihistamines such as diphenhydramine (BENADRYL), antidepressants such as amitriptyline (ELAVIL) -- a Do Not Use drug -- or some antipsychotic drugs such as thioridazine (MELLARIL).
- An increased use of antihypertensive drugs in people with high blood pressure that was caused or increased by very high doses of nonsteroidal anti-inflammatory drugs (NSAIDs), used as painkillers or for arthritis).
Failing to Treat Certain Problems with Nondrug Treatments
Research has shown that many doctors are too quick to pull the prescription trigger. In one study, in which doctors and nurse practitioners were presented with part of a clinical scenario -- as would occur when first seeing a patient with a medical problem -- and then encouraged to ask to find out more about the source of the problem, 65% of doctors recommended that a patient complaining of insomnia be treated with sleeping pills even though, had they asked more questions about the patient, they would have found that the patient was not exercising, was drinking coffee in the evening, and, although awakening at 4 A.M., was actually getting seven hours of sleep by then.
In a similar study, doctors were presented with a patient who complained of abdominal pain and endoscopy showed diffuse irritation in the stomach. Sixty-five percent of the doctors recommended treating the problem with a drug -- a histamine antagonist (such as Zantac, Pepcid, or Tagamet). Had they asked more questions they would have discovered that the patient was using aspirin, drinking a lot of coffee, smoking cigarettes, and was under considerable emotional stress -- all potential contributing factors to abdominal pain and stomach irritation.
In summarizing the origin of this overprescribing problem, the authors stated: "Apparently quite early in the formulation of the problem, the conceptual focus [of the doctor] appears to shift from broader questions like 'What is wrong with this patient?' or 'What can I do to help?' to the much narrower concern, 'Which prescription shall I write?'" They argued that this approach was supported by the "barrage" of promotional materials that only address drug treatment, not the more sensible lifestyle changes to prevent the problem.
In both of the above scenarios, nurse practitioners were much more likely than doctors to take an adequate history that elicited the causes of the problems and, not surprisingly, were only one-third as likely as the doctors to decide on a prescription as the remedy instead of suggesting changes in the patient's habits.
In later discussions about insomnia, high blood pressure, situational depression, mild adult-onset diabetes, and other problems, you will find out about the proven-effective nondrug remedies that should first be pursued before yielding to the riskier pharmaceutical solutions.
Treating Viral Infections with Antibiotics or Treating Other Diseases with Drugs That Are Not Effective for Those Problems
Two recently published studies, based on nationwide data from office visits for children and adults, have decisively documented the expensive and dangerous massive overprescribing of antibiotics for conditions which, because of their viral origin, do not respond to these drugs. Forty-four percent of children under 18 years old were given antibiotics for treatment of a cold and 75% for treatment of bronchitis. Similarly, 51% of people 18 or older were treated with antibiotics for colds and 66% for bronchitis. Despite the lack of evidence of any benefit for most people from these treatments, more than 23 million prescriptions a year were written for colds, bronchitis, and upper respiratory infections. This accounted for approximately one-fifth of all prescriptions for antibiotics written for children or adults. An accompanying editorial warned of "increased costs from unnecessary prescriptions, adverse drug reactions, and [subsequent] treatment failures in patients with antibiotic-resistant infections" as the reasons to try to reduce this epidemic of unnecessary antibiotic prescribing.
Similar misprescribing of a drug useful and important for certain problems, but not necessary or effective -- and often -- dangerous for other problems can be seen in another recent study. In this case, 47% of the people admitted to a nursing home who were taking digoxin, an important drug for treating an abnormal heart rhythm called atrial fibrillation or for treating severe congestive heart failure, did not have either of these medical problems and were thereby being put at risk for life-threatening digitalis toxicity without the possibility of any benefit.
A final example in this category involves the overuse of a certain class of drugs, in this case calcium channel blockers, which have not been established as effective for treating people who have had a recent heart attack. The study shows that this prescribing pattern actually did indirect damage to patients because their use was replacing the use of beta-blockers, drugs shown to be very effective for reducing the subsequent risk of death or hospitalization following a heart attack. Use of a calcium channel blocker instead of a beta-blocker was associated with a doubled risk of death, and beta-blocker recipients were hospitalized 22% less often than nonrecipients.
The Prescribing of More Dangerous and/or Less Effective Do Not Use Drugs Instead of Safer Alternatives
There are 160 drugs listed in this book for which we recommend safer alternatives. Forty-three of these Do Not Use drugs are for heart disease or high blood pressure and make up 39% of all the drugs in the book for these problems. Twenty of the Do Not Use drugs are for treating insomnia, anxiety, depression, or other mental problems, and make up 43% of the drugs in the book for these problems. Another 20 of the Do Not Use drugs are for treating pain, and make up 36% of the drugs in the book for these problems. Thirteen of the Do Not Use drugs are for treating gastrointestinal problems and make up 37% of the drugs in the book for these problems. Twenty-four of the Do Not Use drugs are for treating coughs, colds, allergies, or asthma, and make up 63% of the drugs in the book for these problems. Sixteen of the Do Not Use drugs are for treating infections and make up 28% of the drugs in the book for these problems. Although the original determinations for these Do Not Use drugs were based on their use by older adults, we have concluded that the same warnings apply to use by any adults.
Included in this list of 160 are drugs we label Do Not Use Until Five Years After Release. We have applied this warning to drugs that have only recently appeared on the market, for which there is no evidence of their superiority over older drugs about which we have much more information as to long-term safety and effectiveness. Because of incomplete and worrisome safety information, there is a risk that some of these newer drugs will have to be banned. But by the time they have been on the market for five years, it is much less likely that they will be banned, and it is much more likely that, if they are still being used, there will be much better information about their safety and effectiveness.
Another category of drugs that is misprescribed even though there are safer alternatives, are drugs to which patients are known to be allergic, but which their physicians have not taken a careful medical history about.
The Causes of Misprescribing and Overprescribing: Drug Companies, the FDA, Doctors, Pharmacists, and Inadequately Informed or Not-Vigilant-Enough Patients
The Drug Industry
The primary culprit in promoting the misprescribing and overprescribing of drugs is the pharmaceutical industry, which now sells about $80 billion worth of drugs in the United States alone. By intimidating the Food and Drug Administration (FDA) into approving record numbers of me-too drugs (drugs that offer no significant benefit over drugs already on the market) that often have dangerous adverse effects and by spending well in excess of $12 billion a year to promote drugs, using advertising and promotional tricks that push at or through the envelope of being false and misleading, this industry has been extremely successful in distorting, in a profitable but dangerous way, the rational processes for approving and prescribing drugs. Two studies of the accuracy of ads for prescription drugs widely circulated to doctors both concluded that a substantial proportion of these ads contained information that was false or misleading and violated FDA laws and regulations concerning advertising.
The fastest-growing segment of drug advertising is directed not at doctors but at patients. It has been estimated that from 1991 to 1998, DTC (direct-to-consumer) advertising expenditures in the United States grew from about $60 million a year to $1.5 billion a year, an increase of 25-fold in just seven years, employing misleading advertising campaigns similar to those used for doctors. A recent study by Consumer Reports of 28 such ads found that "only half were judged to convey important information on side effects in the main promotional text," only 40% were "honest about efficacy and fairly described the benefits and risks in the main text," and 39% of the ads were considered "more harmful than helpful" by at least one reviewer. This campaign has been extremely successful. According to a drug industry spokesman, "There's a strong correlation between the amount of money pharmaceutical companies spend on DTC advertising and what drugs patients are most often requesting from physicians." The advertising "is definitely driving patients to the doctor's office, and in many cases, leading patients to request the drugs by name." The problems with DTC advertising are best summed up in an article written by a physician ten years ago in The New England Journal of Medicine, before the current binge had really begun: "If direct [to consumer] advertising should prevail, the use of prescription medication would be warped by misleading commercials and hucksterism. The choice of a patient's medication, even of his or her physician, could then come to depend more on the attractiveness of a full-page spread or prime-time commercial than on medical merit...such advertising would serve only the admakers and the media, and might well harm our patients."
The Food and Drug Administration (FDA)
Attempting to fend off FDA-weakening legislation even worse than that which was signed into law in 1997, the FDA has bent over backwards to approve more drugs, culminating in 1996 and 1997 when the agency approved a larger number than had ever been approved in any two-year period. Thousands of people were injured or killed after taking one of three such recently approved drugs (which have subsequently been recalled from the market). These drugs were the weight loss drug dexfenfluramine (REDLUX), a heart drug mibefradil (POSICOR), and the painkiller bromfenac (DURACT). Other drugs that would not have gotten approved in a more cautious era at the FDA have also been approved, but are likely either to be banned or to be forced to carry severe warnings that will substantially reduce their use. Many of these are included in this book and listed as Do Not Use drugs.
In the 27 years since the Public Citizen's Health Research Group started monitoring the FDA and the drug industry, the current pro-industry attitude at the FDA is as bad and dangerous as it has ever been. In addition to record numbers of approvals of questionable drugs, FDA enforcement over advertising has fallen behind. The division at FDA responsible for policing prescription drug advertising has not been given adequate resources to keep up with the torrent of newly approved drugs. As a result, the drug industry correctly believes it can get away with more violative advertising than in the past. The role of the U.S. Congress in pushing the FDA into approving more drugs, and passing, with the FDA's reluctant approval, legislation to further weaken the FDA's ability to protect the public, cannot be overlooked.
Physicians
The well-financed promotional campaigns by drug companies would not have as much of an impact as they do were there not such an educational vacuum about proper prescribing of drugs, a serious problem that must be laid at the feet of medical school and residency training. The varieties of overprescribing and misprescribing of drugs by doctors -- the seven all-too-often-deadly sins of prescribing -- are all strongly enhanced by the mind-altering properties of drug promotion. The best doctors, of whom there are many, do not waste their time talking to drug sales people, toss promotional materials away, and ignore drug ads in medical journals. Too many other doctors, however, are heavily influenced by drug companies, accepting free meals, free drinks, and free medical books in exchange for letting the drug companies "educate" them at symposia in which the virtues of certain drugs are extolled. Unfortunately, many of these doctors are too arrogant to realize that there is no such thing as a free lunch. The majority of doctors attending such functions have been found to increase their prescriptions for the targeted drugs following attendance at the "teach-in."
Beyond traditional advertising and promotion and their influence, bias of drug-company-sponsored research, as published in medical journals, also can sway doctors toward more favorable impressions about drugs. An analysis was done of 56 trials that were paid for by drug companies and reported in 52 medical journals about drugs for arthritis and pain -- non-steroidal anti-inflammatory drugs (NSAIDs). (These drug-company-sponsored studies represented 85% of those that the researchers originally looked at.) In studies identifying the company's drug as less toxic than another drug, in barely one-half of the studies was there justification for the finding of less toxicity. This certainly explains why, contrary to fact, newer arthritis drugs almost always "seem" safer than older, usually much less expensive ones.
A final example demonstrates the ignorance of many physicians, especially in dealing with prescribing drugs to older adults. A study of physicians who treat Medicare patients found that 70% of the doctors who took an examination concerning their knowledge of prescribing for older adults failed to pass the test. The majority of physicians who were contacted for participation in the study refused to take the test, often giving as their reason that they had a "lack of interest in the subject." The authors concluded "many of these physicians [who failed the exam] had...not made good use of the best information on prescribing for the elderly."
Pharmacists
A small fraction of pharmacists have, in our view, betrayed their professional ethics and are working for drug companies, engaging in such activities as calling doctors to get them to switch patients from drugs made by a company other than the one the pharmacist works for to the pharmacist's employer's drugs. In addition, pharmacy organizations such as the American Pharmaceutical Association and others have fought hard to prevent the FDA from requiring accurate patient package information to be dispensed with each prescription filled.
Too many pharmacists, despite having computers to aid them, have been willing to fill prescriptions for pairs of drugs which, because of life-threatening adverse drug interactions if used at the same time, should never be dispensed to the same person.
- Sixteen (32%) of 50 pharmacies in Washington, D.C., filled prescriptions for erythromycin and terfenadine (SELDANE) without comment. These two drugs, if used in combination, can cause fatal heart arrhythmias.
- In another study, of 245 pharmacists in seven cities, about one-third of pharmacists, did not alert consumers to the potentially fatal and widely publicized interaction between Hismanal, a common antihistamine, and Nizoral, an often-prescribed antifungal drug. Only 4 out of 17 pharmacists warned of the interaction between oral contraceptives and Rimactane, an antibiotic that could decrease the effectiveness of the oral contraceptive. Only 3 out of 61 pharmacists issued any verbal warnings about the interaction between Vasotee and Dyazide -- two drugs for treating hypertension -- which may lead to dangerously high levels of potassium in the blood.
- In yet another study, concurrent use of terfenadine (SELDANE) and contraindicated drugs declined over time. The rate of same-day dispensing declined by 84%, from an average of 2.5 per 100 persons receiving terfenadine in 1990 to 0.4 per 100 persons during the first six months of 1994, while the rate of overlapping use declined by 57% (from 5.4 to 2.3 per 100 persons). Mostcases involved erythromycin. Despite substantial declines following reports of serious drug-drug interactions and changes in product labeling, concurrent use of terfenadine and contraindicated antibiotics such as erythromycin and clarithromycin (BIAXIN) and antifungals such as ketoconazole (NIZORAL) continued to occur.
Patients
For too many patients, the system is stacked against you -- drug companies, doctors, and pharmacists are too often making decisions that ultimately derive from what is best for the drug companies, doctors, and pharmacists, and not necessarily from what is best for you. This book has been researched and written to help you come out ahead in the struggle with our health care industry.
In Chapter 2, concerning adverse drug reactions, you can learn which common medical problems -- depression, insomnia, sexual disorders, parkinsonism, falls and hip fractures, constipation, and many others -- can actually be caused by drugs. Once you recognize these problems, you can take care of yourself and your family and bring the problems to an end by discussing safer alternatives with your physician.
Chapter 3, the largest section of the book, discusses 456 drugs, including 160 that we and our consultants think you should not use. For each of these, we recommend safer alternatives. In addition, Chapter 3 lists hundreds of drug combinations that should not be used because of serious interactions.
Chapter 4 presents a detailed strategy, beyond information on specific adverse effects and drugs, to help you to use drugs more safely, including Ten Rules for Safer Drug Use and how to use and maintain your own Drug Worksheet for Patient, Family, Doctor and Pharmacist. This is your personalized plan for avoiding becoming a victim of overprescribing or misprescribing.
Chapter 5 discusses the latest information about generic drugs and shows you how and why you can and should save hundreds of dollars a year or more.
In short, this book is intended to help you and your family to improve your health by using drugs, if necessary, more carefully and recognizing those you should avoid.
Copyright © 1999 by Public Citizen Foundation, Inc., Sidney M. Wolfe, M.D., and the Public Citizen's Health Research Group
Product Details
- Publisher: Pocket Books (April 14, 2009)
- Length: 960 pages
- ISBN13: 9781439138809
Browse Related Books
Resources and Downloads
High Resolution Images
- Book Cover Image (jpg): Worst Pills, Best Pills eBook 9781439138809(5.5 MB)